Skin and Adnexal Tumors
Skin and Adnexal Tumors
Skin and Adnexal tumors encompass a diverse group of growths arising from the epidermis, dermis, or adnexal structures such as hair follicles, sweat glands, and sebaceous glands. While the majority are benign, some can be locally aggressive or malignant, requiring specialized management.
Common benign entities include dermatofibroma, pilomatricoma, trichilemmoma, sebaceous adenoma, syringoma, and hidradenoma. These often present as slow-growing nodules or papules on the face, scalp, trunk, or extremities.
Malignant skin and adnexal tumors, though rare, include dermatofibrosarcoma protuberans (DFSP), microcystic adnexal carcinoma, sebaceous carcinoma, and eccrine porocarcinoma. DFSP is notorious for local infiltration and high recurrence if inadequately excised. Sebaceous carcinoma, often around the eyelids, can be aggressive and metastasize.
Dr. Pradeep Kumar, with his musculoskeletal oncology expertise extended to complex soft tissue tumors of the skin and extremities, offers precise diagnosis through clinical examination, dermoscopy, advanced imaging, and biopsy with immunohistochemical staining for accurate subtyping.
Treatment is tailored:
- Wide local excision with confirmed margins for malignant and aggressive benign tumors.
- Mohs micrographic surgery collaboration for cosmetically sensitive areas.
- Reconstruction using skin grafts or flaps to preserve function and aesthetics.
- Sentinel lymph node biopsy and systemic therapy for high-risk cases.
Early intervention ensures excellent outcomes with minimal morbidity. Any persistent, changing, or ulcerating skin lesion warrants prompt specialist evaluation—timely expert care provides cure and optimal cosmetic results.
Treatment is tailored:
- Wide local excision with confirmed margins for malignant and aggressive benign tumors.
- Mohs micrographic surgery collaboration for cosmetically sensitive areas.
- Reconstruction using skin grafts or flaps to preserve function and aesthetics.
- Sentinel lymph node biopsy and systemic therapy for high-risk cases.
Early intervention ensures excellent outcomes with minimal morbidity. Any persistent, changing, or ulcerating skin lesion warrants prompt specialist evaluation—timely expert care provides cure and optimal cosmetic results.
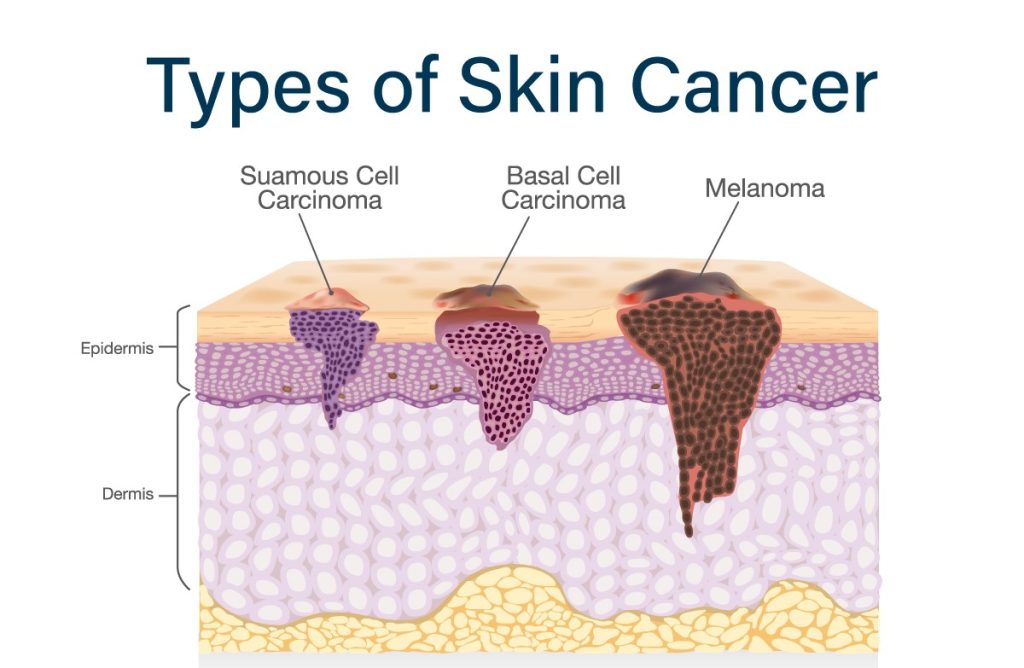
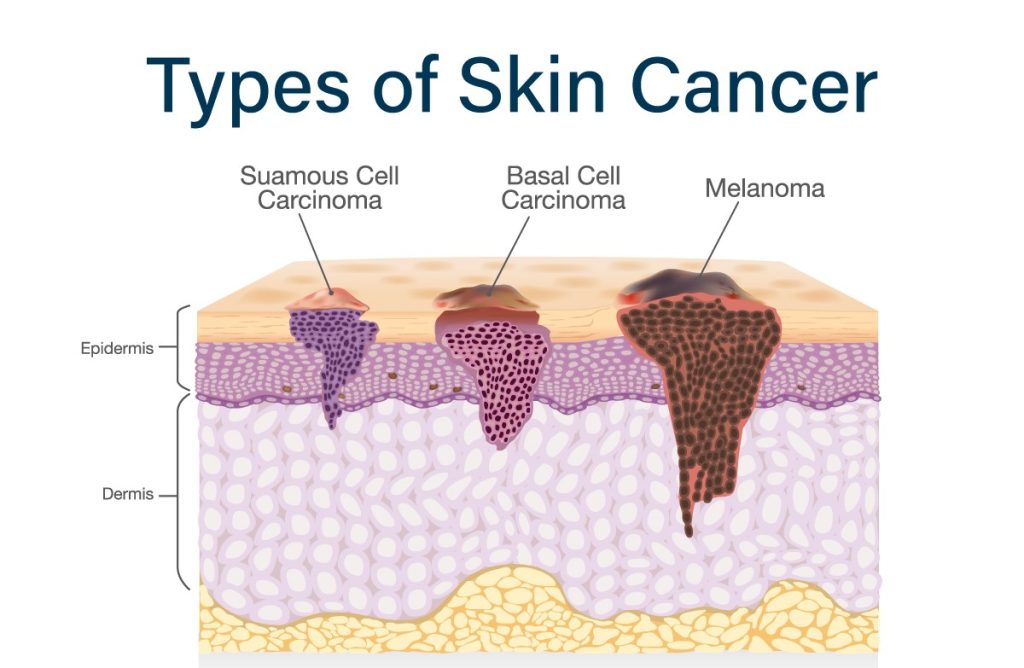
Squamous Cell Carcinoma

Squamous cell carcinoma (SCC) is the second most common skin cancer, arising from squamous cells in the outer epidermis layer. Primarily caused by cumulative UV exposure, it often appears on sun-exposed areas like the face, ears, neck, and hands as a red, scaly patch, firm bump, or non-healing sore.
While usually slow-growing, SCC can become invasive, spreading to lymph nodes or distant sites if untreated—especially in immunocompromised patients. Risk factors include fair skin, older age, and actinic keratoses (precancerous lesions).
Diagnosis involves biopsy; treatment options range from excision, Mohs surgery, radiation, to systemic therapy for advanced cases. Early detection ensures high cure rates exceeding 95%. Regular skin checks and sun protection are vital for prevention.

Melanoma
Melanoma
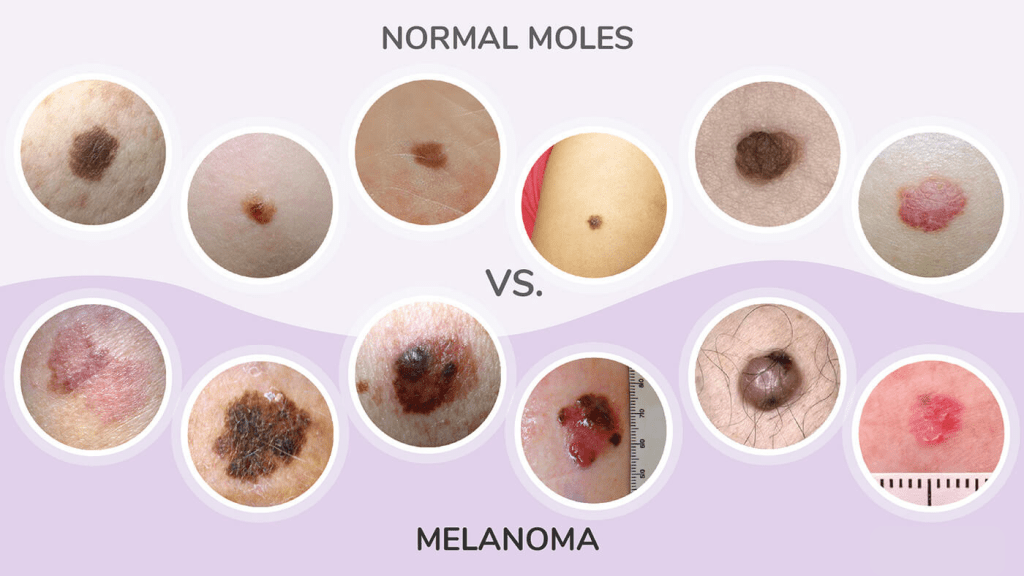
Melanoma is the most dangerous skin cancer, originating from melanocytes—the pigment-producing cells. Though less common than non-melanoma types, it causes most skin cancer deaths due to its potential to metastasize early.
It often presents as an asymmetrical mole with irregular borders, varied colors (black, brown, blue), diameter >6mm, or evolving changes (ABCDE rule). UV exposure, fair skin, many moles, and family history increase risk.
Staging via biopsy and sentinel node assessment guides treatment: surgery for early stages, immunotherapy, targeted therapy (e.g., BRAF inhibitors), or chemotherapy for advanced. Survival rates are excellent (>99%) when caught early but drop significantly with metastasis. Self-exams and dermatologist visits are crucial.
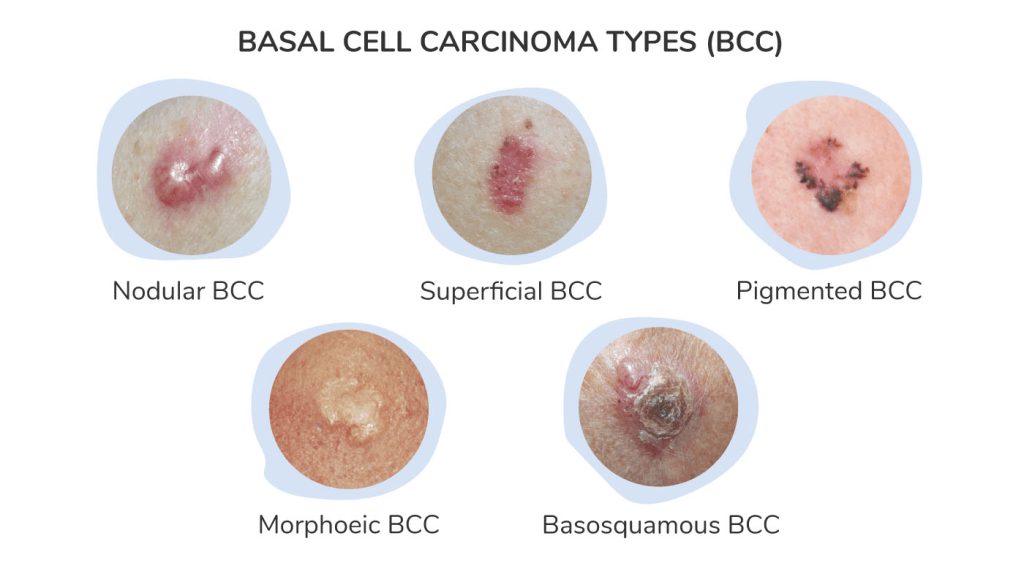
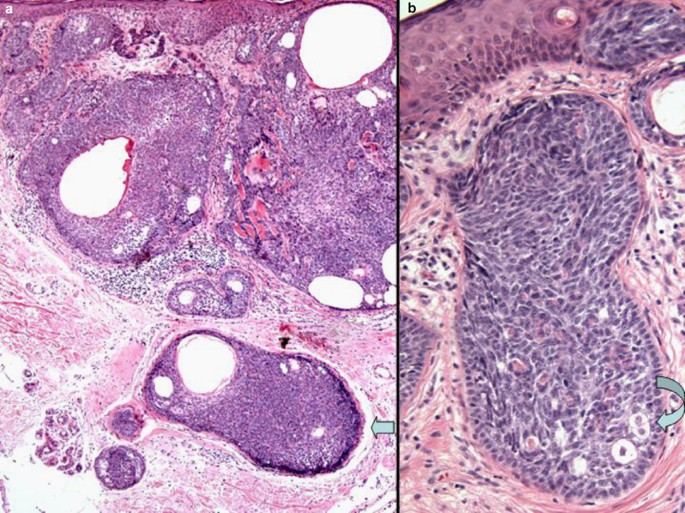
Basal Cell Carcinoma
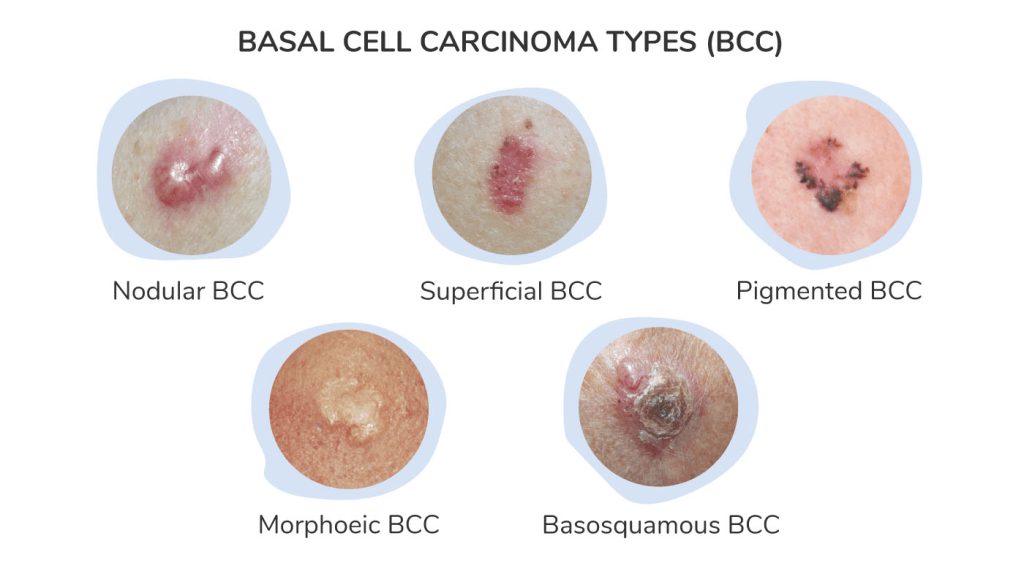
Basal cell carcinoma (BCC) is the most common skin cancer, developing from basal cells in the epidermis’s lower layer. Linked to intense or prolonged UV exposure, it typically appears on sun-exposed sites like the face as a pearly nodule, shiny bump, or pink patch that may bleed or crust.
BCC grows slowly and rarely metastasizes but can cause local destruction if ignored. Subtypes include nodular, superficial, and morpheaform (aggressive).
Risk factors: fair skin, older age, radiation history. Diagnosis via biopsy; treatments include excision, Mohs micrographic surgery (ideal for facial areas), curettage, cryotherapy, or topical creams for superficial cases. Cure rates approach 99% with early intervention. Prevention emphasizes sunscreen and avoiding peak sun hours.
Other Skin Adnexal Neoplasms
Other Skin Adnexal Neoplasms
Skin adnexal neoplasms are rare tumors arising from hair follicles, sebaceous, or sweat glands. Malignant forms, like microcystic adnexal carcinoma, porocarcinoma, or sebaceous carcinoma, are aggressive with local invasion and occasional metastasis.
They present as slow-growing nodules, often on the head/neck, mimicking benign lesions. Risk factors include UV, radiation, or genetic syndromes.
Diagnosis requires biopsy with immunohistochemistry for subtyping. Treatment involves wide excision, sometimes Mohs surgery, radiation, or lymph node evaluation. Recurrence is common in aggressive types like microcystic adnexal carcinoma due to perineural spread.
Outcomes vary; early specialized care improves prognosis. Any persistent or unusual skin growth warrants prompt evaluation by a dermatologist or oncosurgeon.